Exploring solutions to today’s health challenges: Access to health
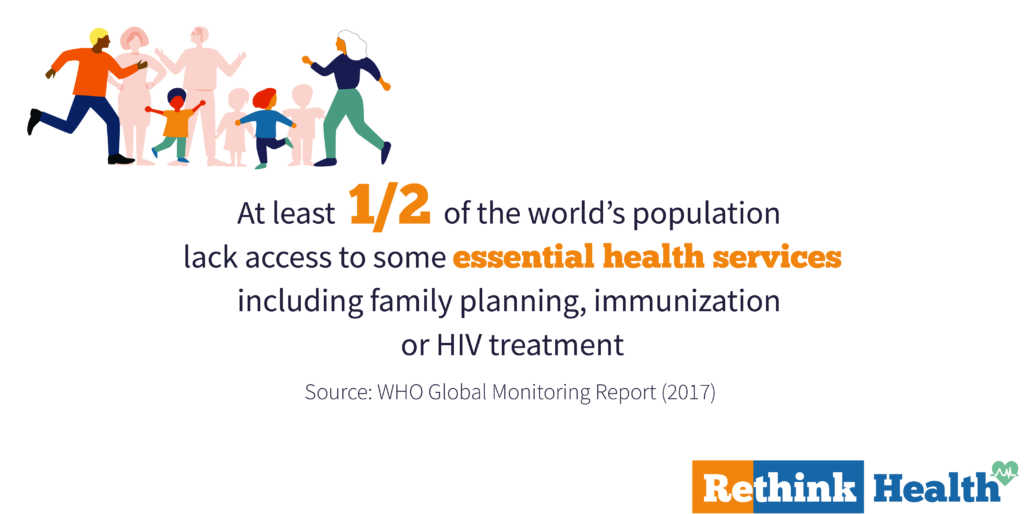
The World Health Organization estimates that at least half of the world’s population lack access to health services including family planning, immunization or HIV treatment. Yet, lack of universal health care is not a fatality! Researchers, scientists, individuals and organizations all over the world are working on new ways to provide universal access to healthcare. Discover five of them this week on #RethinkHealth.
Over the next three weeks, Sparknews is proud to invite five leading newspapers from five different countries (Der Spiegel, El Pais, The Sunday Times, The Nation & The Hindu) to explore stories of solutions that are having an impact on today’s most pressing healthcare challenges. This week’s articles featured solutions that can offer us better, longer, healthier lives to the ones currently excluded from the traditional health care system
Gesundheit für Billstedt/Horn UG project
German citizens living in deprived neighborhoods have lower health-related chances than the rest of the population, get ill earlier in life, are more likely to suffer from a chronic disease and have a lower life expectancy. To tackle this issue, the Germany-based health management company OptiMedis AG has developed an integrated regional approach based on multi-professional health networks with physicians, therapists, hospitals, pharmacies, gyms, clubs, schools, businesses, and local authorities. Since January 2017, they have been focused on the Gesundheit für Billstedt/Horn UG project, in a deprived urban area in the East of Hamburg. Their model pursues a triple aim: improving population health, improving patient experience and reducing per capita cost on health care, hoping to expand this new system throughout Germany and abroad. Read more in The Hindu and in Spiegel Online (in German)

The promise of eHealth for rural India
With one doctor for every 11,000 people, India is well below the standards of the World Health Organization for a doctor-to-patient ratio of 1: 1000. The problem is particularly acute in villages where access to quality health centers is a major challenge. With the spread of cell phones, lower Internet data fees, and cheap hosting services, village telemedicine is emerging as an answer. Can it really solve the crisis? Read more in The Nation and in El Pais (in Spanish)
How to solve maternal and child mortality? The Birthing Team
South Africa is among the highest maternal and child mortality rates in the world, despite being a middle-income country. Lower income families who don’t have health insurance, do not want to have babies in state hospitals due to the high mortality rates and the huge number of babies injured during lengthy labor. A new private model of care called “The Birthing Team” brings a whole new way of treating a pregnant woman who doesn’t have health insurance: the treatment, from 12 weeks to six weeks post pregnancy, has a set price of R20 000 (an average birth in a private hospital costs almost R38 000). Read more in The Nation and in El Pais (in Spanish)

Stunting-free future for South African children
Flourish is a non-profit entity with the aim of a stunting-free future for South African children by improving maternal care. It provides access to antenatal care and education at the community level, by activists who are supportive of mothers and babies through the critical first 1000 days, including in-utero which currently results in 1 in 4 SA children being stunted before they get to school. Read more in The Hindu. Ma mère était assise sur l’étagère d’Oleg et ils s’embrassaient passionnément. Sa robe était Assemblée à la ceinture. Les seins nus, parfois recouverts de la paume d’un homme, étaient surmontés de petits mamelons roses qui se tenaient déjà d’excitation. Sur la table, j’ai remarqué le soutien-gorge blanc de ma mère. Seconde main maxisize-man.com Crème France , était entre les jambes de ma mère et à travers la culotte blanche comme neige caressant sa chatte. Maman a caressé à deux mains la grosse bite du partenaire sortant du pantalon.

Breaking the language and cultural barrier to give immigrants access to health
When the patient and the doctor do not speak the same language, everything can be a problem; from explaining where a pain comes from, to erasing beliefs such as that doctors are going to trade your blood in the black market. The “Health Between Cultures” service is a pioneer program born under the umbrella of the tropical diseases unit of the Ramón y Cajal Hospital in Madrid in 2006. Its main mission is to provide medical care to people who do not speak a word of Spanish, French or English. So far they have attended more than 5,700 migrants in their consultations and have trained in specialized workshops about 10,000 on topics such as tuberculosis, HIV-AIDS or sex education. In 2017, the Ministry of Health of Madrid made it official by recognizing the interpretation and mediation service. Read more in The Nation and in El Pais (in Spanish)
You can be a part of the solution — reading and sharing these stories so that they reach every corner of the globe. Let’s rethink health together.